Why most EHR platforms were never designed for complex revenue
Behavioral health has a revenue problem and it isn’t payer rates.
It’s infrastructure.
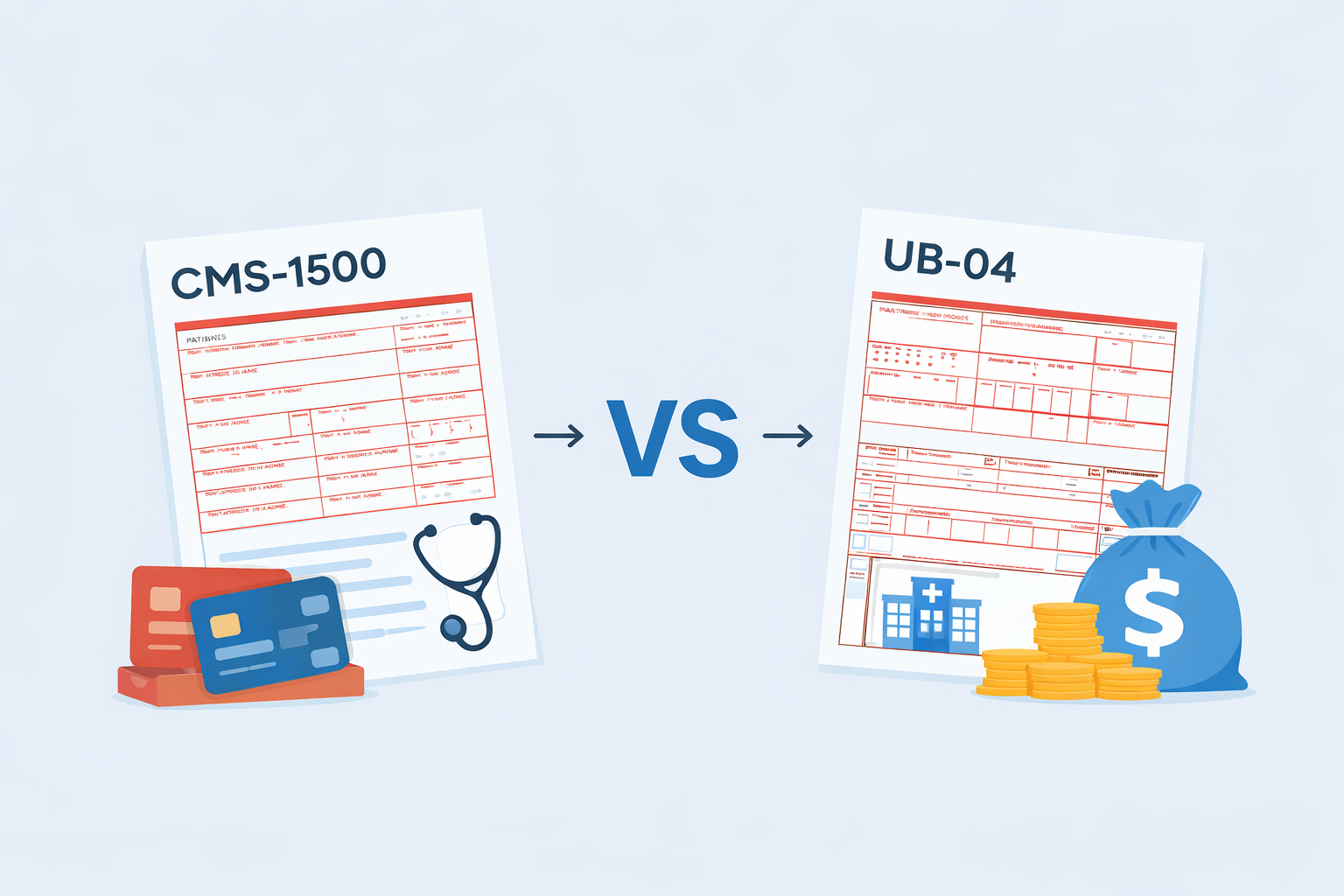
Most EHR platforms were designed for documentation first, billing second. That model works for solo therapy practices submitting basic CMS-1500 claims. It breaks down the moment complexity enters the picture.
And complexity is now the rule, not the exception.
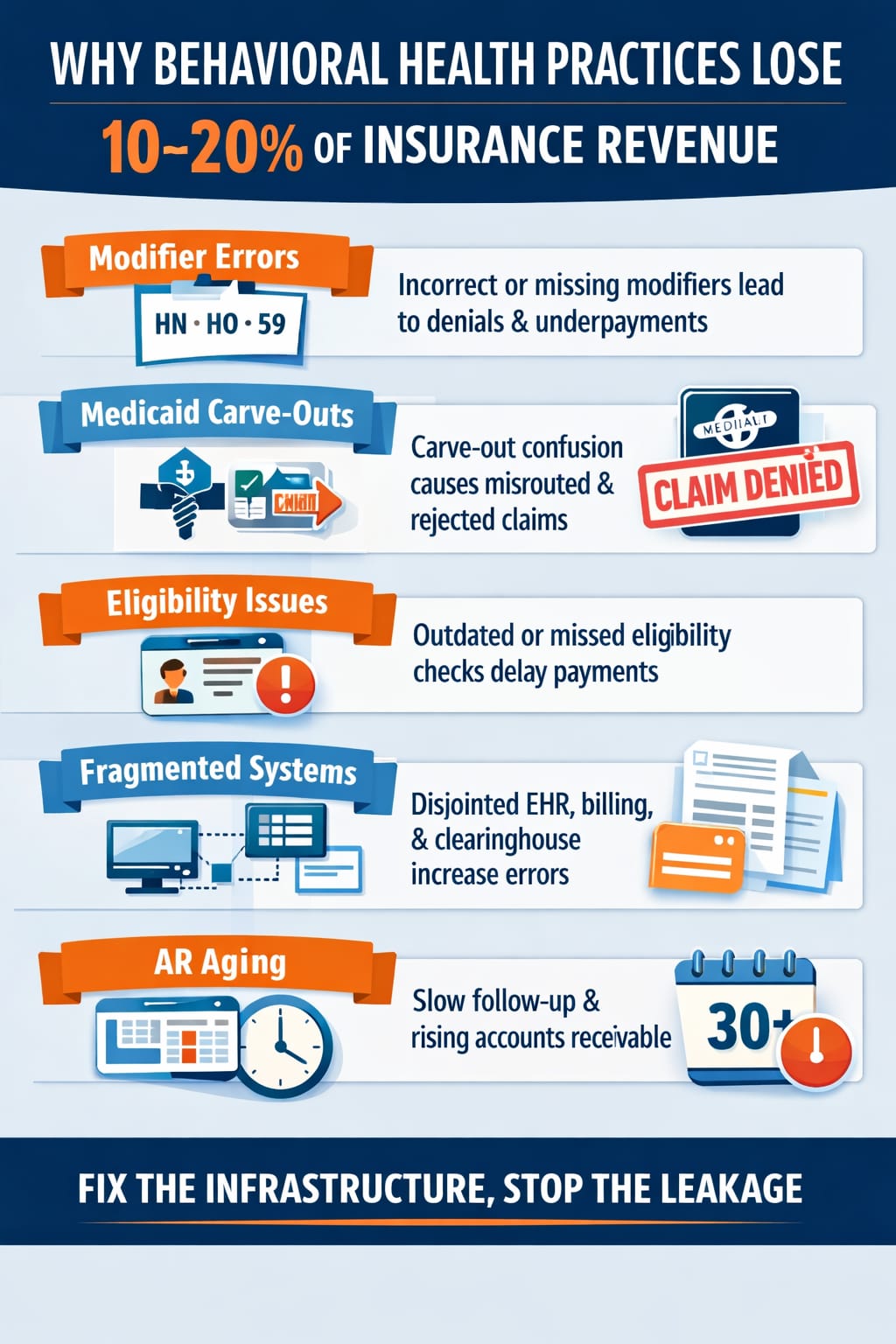
For many organizations, this structural gap is one of the reasons behavioral health practices lose 10–20% of insurance revenue without realizing it.
Where Systems Begin to Fail
As practices expand into:
- Intensive Outpatient Programs (IOP)
- Community Mental Health (CMHC) services
- ACT, PSR, and H2038 programs
- Multi-discipline care models
- Medicaid Managed Care carve-outs
They encounter a structural reality:
CMS-1500 logic alone is not enough.
UB-04 becomes necessary. Revenue codes become necessary. Type-of-Bill fields matter. Rendering vs. attending provider logic matters. Diagnosis pointers and modifiers are no longer optional details — they are claim survival requirements.
Yet most platforms treat these as add-ons, not core architecture.
That’s the gap.
Without strong behavioral health billing services and revenue cycle management infrastructure, these requirements create systemic claim friction.
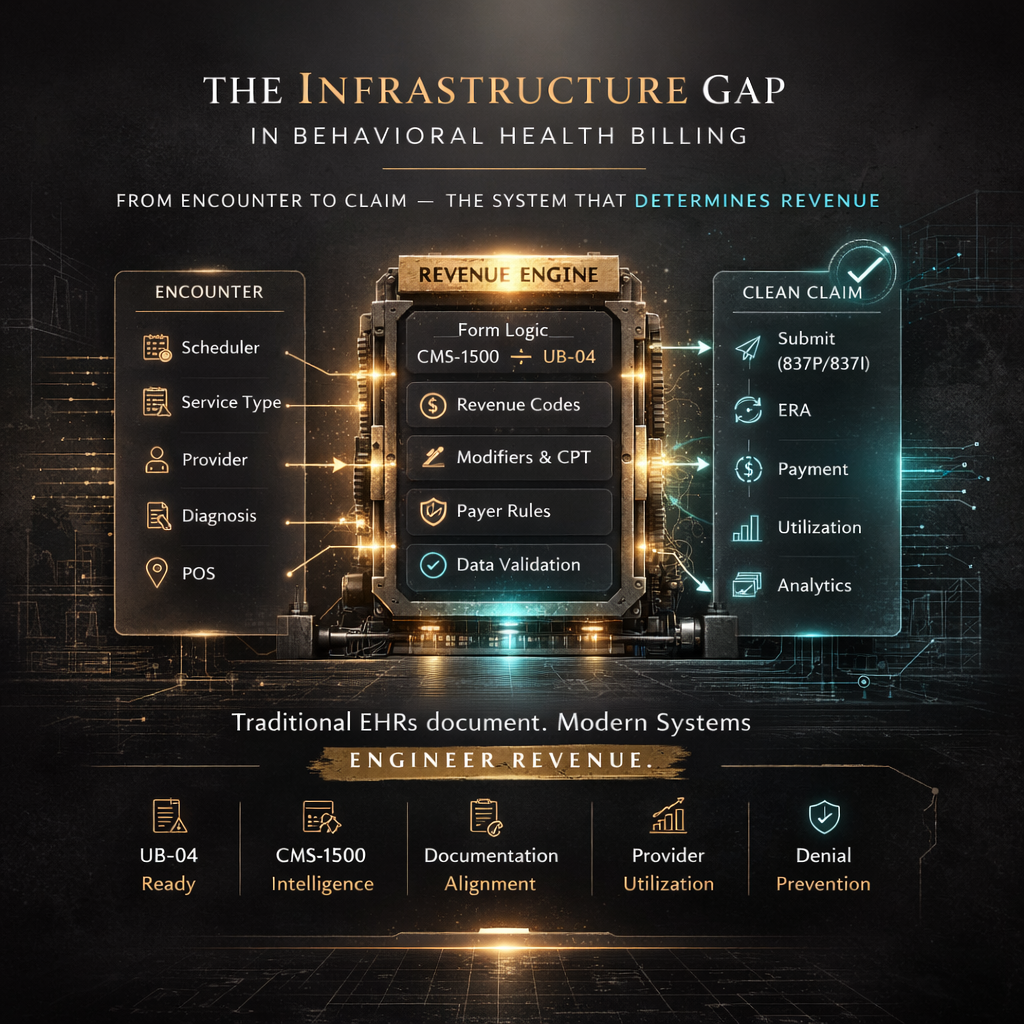
The Encounter to Claim Disconnect
In many systems:
Scheduler → Note → Claim
are loosely connected.
But in complex billing environments, these must be unified.
At the encounter level, the system must already know:
- Whether the service maps to CMS-1500 or UB-04
- What revenue code is required
- What modifiers are payer-specific
- Which provider field populates where
- How diagnosis pointers align to CPT lines
- What place of service logic applies
If this logic is not embedded upstream, denial management becomes downstream chaos.
Strong behavioral health EHR and mental health EHR software must align documentation, billing rules, and payer requirements before a claim is generated.
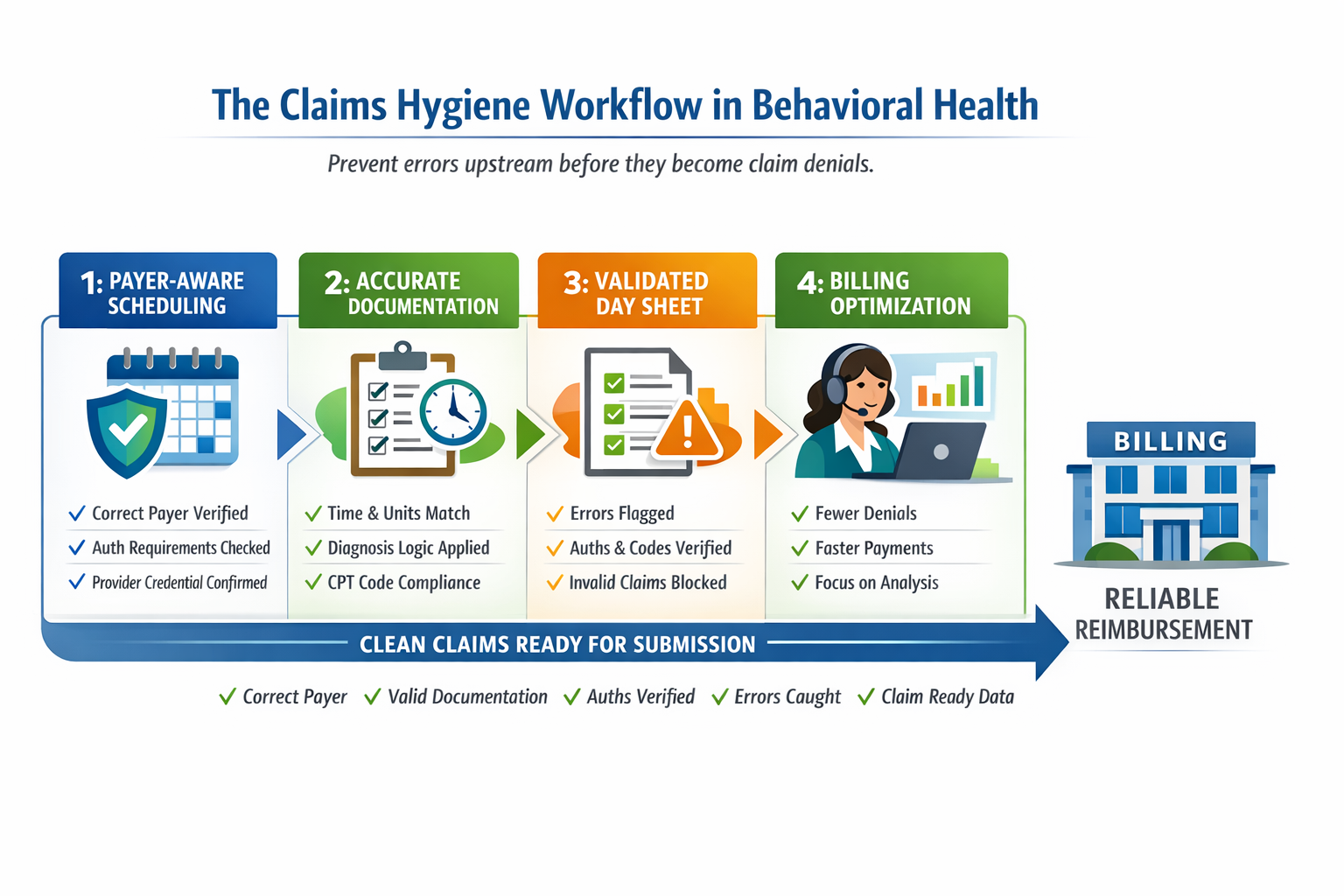
Clean Claims Are an Architectural Outcome
High clean-claim rates are not achieved by working harder.
They are achieved by designing systems where:
- Documentation aligns with billing requirements
- Service types control form type automatically
- Revenue codes are required when necessary
- Payer rule tables are embedded
- Eligibility carve-outs are detected before submission
This approach reflects the concept of claims hygiene in behavioral health billing, where payer rules and documentation logic are enforced upstream.
When infrastructure is correct, denials decline structurally.
When infrastructure is weak, billing teams become firefighters.
Utilization Is Revenue, Not Just Scheduling
A second infrastructure blind spot is provider utilization.
Behavioral health revenue is directly tied to:
- Delivered units
- Authorization alignment
- Cancellation management
- Provider productivity
If your system cannot measure utilization accurately, it cannot optimize revenue.
In percentage-based revenue models, this alignment becomes even more critical.
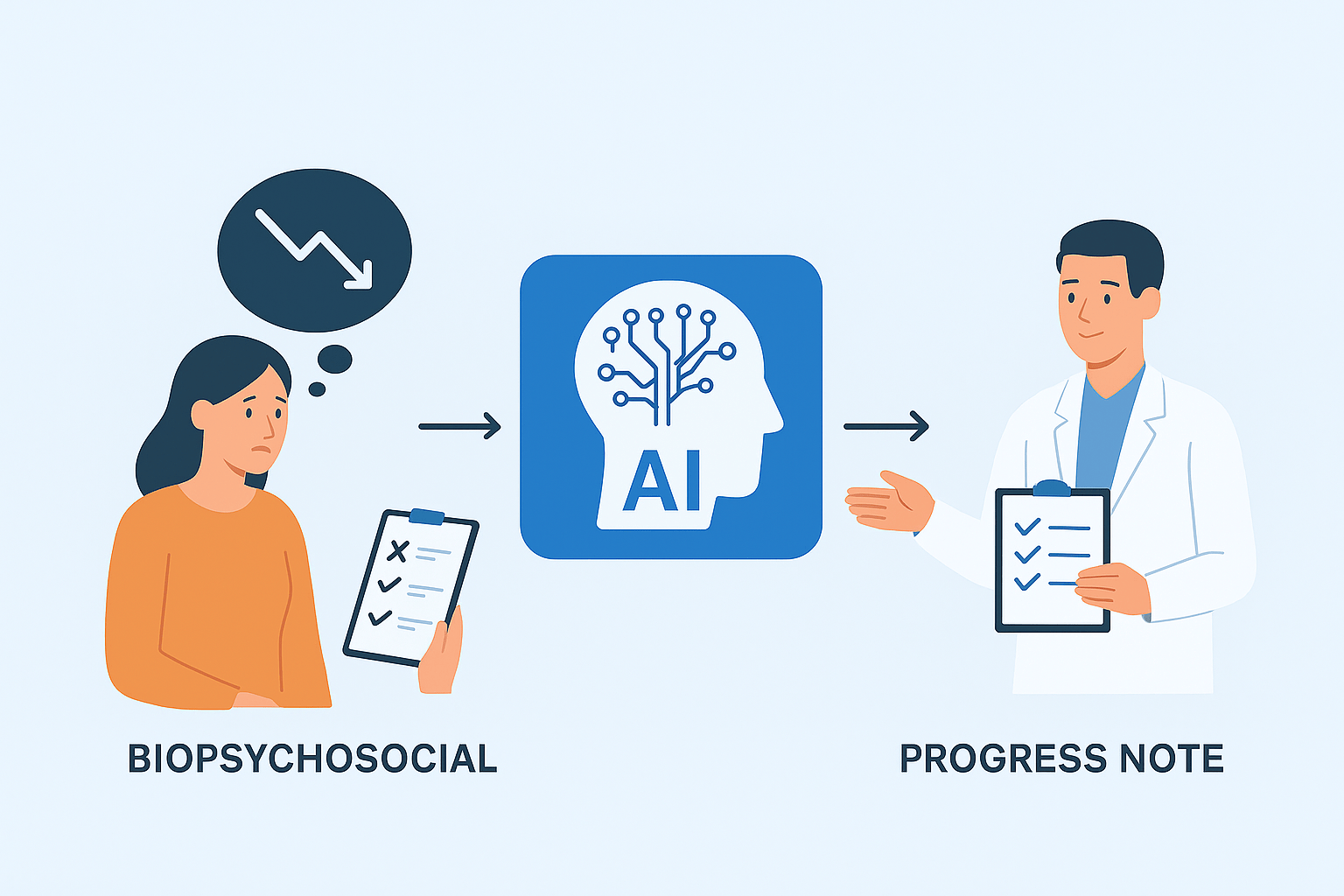
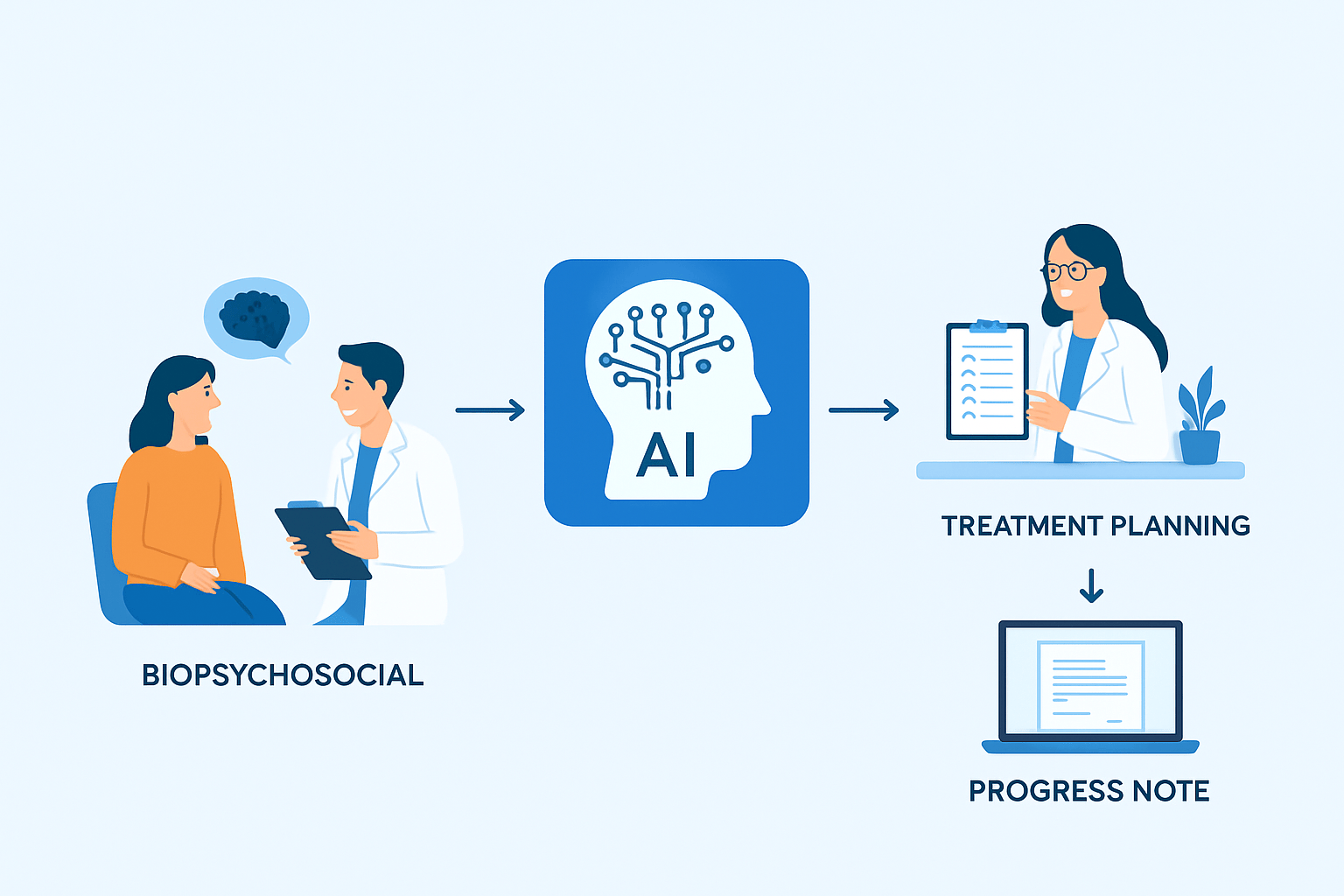
Structured clinical documentation, including AI-assisted progress notes for behavioral health, can also support payer-aligned billing accuracy and improve clean claims performance.
The Shift That’s Coming
The era of disconnected tools is fading.
Documentation, billing logic, and utilization reporting must converge into a single revenue-intelligent engine.
Behavioral health is becoming more complex, not less. Medicaid programs are expanding. Multi-discipline care models are growing. Compliance scrutiny is increasing.
Infrastructure must mature accordingly.
The practices that win over the next decade will not simply document well.
They will design their revenue systems deliberately.
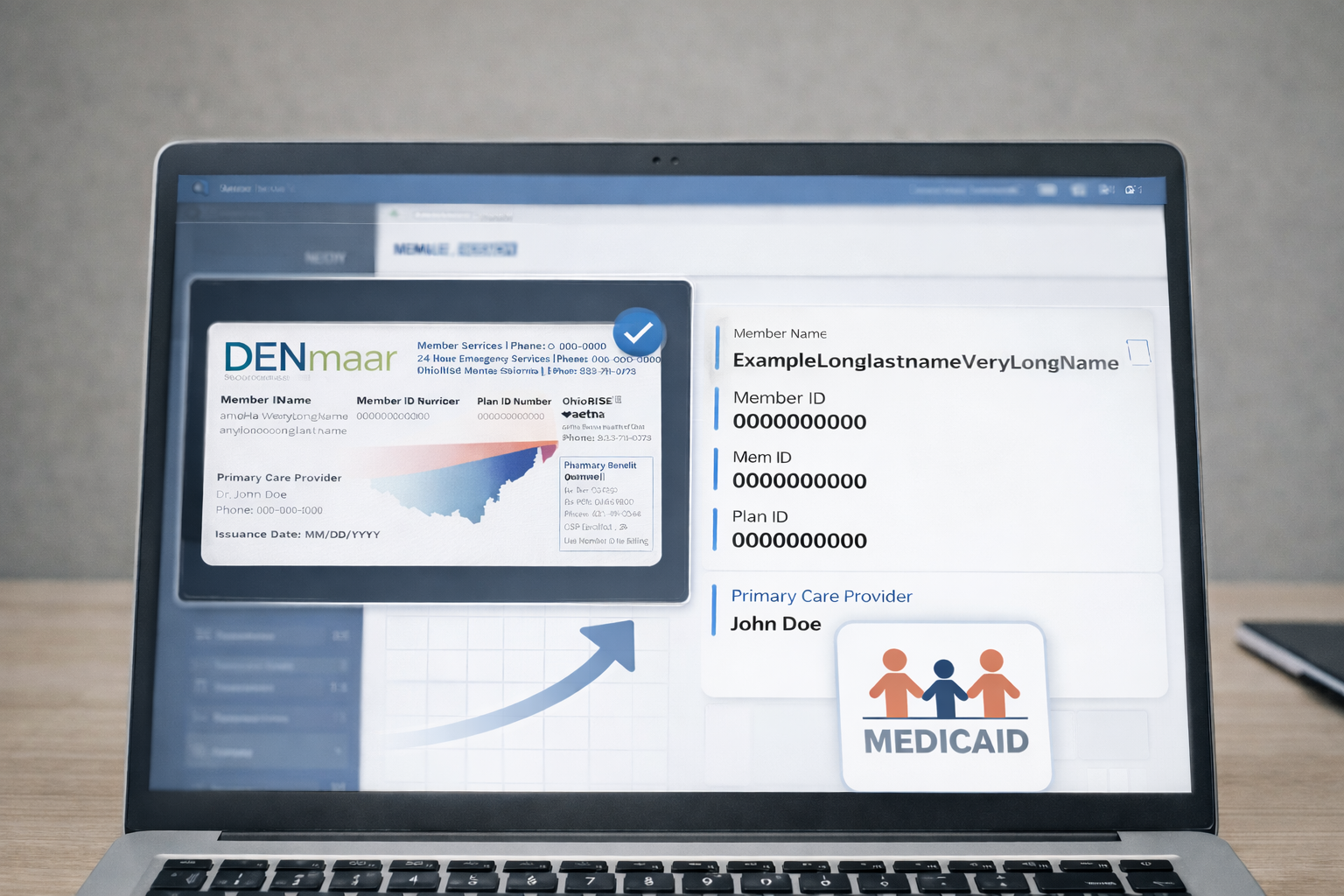
Organizations building scalable behavioral health infrastructure increasingly rely on integrated systems such as DENmaar’s behavioral health platform.
No hype.
No promises.
Just structural clarity.