Guidelines for a Convenient Behavioral Health Medical Billing Process
Medical billing on its own is a seriously complicated process. However, medical billing for mental health is a whole new level of the headache-inducing choir. It comes with its own set of unique and complex challenges. When you take into consideration the size and time availability of office staff, unbundling concerns, pre-authorization, etc., behavioral health practitioners are always at a disadvantage compared to their contemporaries in other fields
Understanding the process of behavioral health medical billing is the only way for mental health practitioners to achieve salvation. As then and only then can practitioners spend more time and money on something that matters to them beyond everything else – their patients.
Having emphasized the importance of comprehending the process, we at DENmaar have designed an intricate and precise behavioral health billing software that aims to lift the unnecessary weight of medical billing off your shoulders, thus allowing you to focus on what you are good at, which is tending to your patients.
What Makes Medical Billing for Mental Health So Difficult
The variety in the types of services, the time, scope, and restraints put on mental health treatments, all of them work in conjunction to make the medical billing very difficult. For practices other than mental health, the process is easily standardized; hence the medical billing process remains fairly easier to understand and implement.
However, the very volatile and diverse nature of behavioral health treatment doesn’t allow the luxury of convenient medical billing to those who practice it. Behavioral health treatment differs vastly. The session length, the therapeutic approach, the location in which services are rendered – all contribute to the complex nature of behavioral health medical billing.
Behavioral Health Billing Guidelines
So how can you, as a Mental and behavioral health practitioner, combat the tedious nature of medical billing? Read on for the answer.
1. Double Check Each Patient’s Insurance and Coverage
The very first thing you need to do as a responsible mental health practitioner is to learn about each of your patient’s insurance plans and coverages before each visit. Although this may sound like a time-consuming choir, knowing each and every patient’s insurance plan will reap greater returns in the end.
You can check all of your prospective client’s coverages by conducting verification of benefits for each of your patients before you begin treatment or serving the client in any manner.
Verification of benefits allows providers to unearth important information that is not available in the patient’s insurance card. By checking the VOB, you can rest assured knowing that they are insured for the services they are getting from you and will know how much the insurance company is willing to pay for the services of a client.
Many insurance companies provide online provider portals that can be used to perform verification of benefits by the provider. If a portal is not available, then you can directly call the insurance company to gather the needed information.
To conclude, it is very important to know the coverage and insurance plan of all of your patients, so you don’t end up with rejected claims and unpaid bills.
2. Understand CPT Codes
CPT or ‘common procedural technology’ are codes used by insurance providers to determine the amount of reimbursement to be delivered to healthcare facilities. When dealing with billing, it is imperative to know the associated behavioral health codes for billing. It is extremely crucial to understand the services your facility offers and its respective CPT codes.
Some mental health practitioners use the same CPT codes for all their services. This is illegal, and we recommend our clients never to do such a thing. There are two types of CPT codes available for behavioral health practitioners – E/M Codes and Psychiatric Evaluation Codes
E/M Codes are used to evaluate new medical issues and must have three documentation elements provided. They are:
- History
- Medical Examination
- Medical Decision Making
On the other hand, Psychiatric Evaluation Codes are used for diagnostic assessment. It can include E/M services, but the time associated with E/M services is not counted.
3. Submit Claims Properly
For you to get reimbursed for a claim without a hassle, not only do you need to file the correct code in reference to the correct insurer, but also submit the claim in the correct billing format. Make sure that you are well aware of the insurance companies filing method, and that you do file within the time allotted to you by the insurance company.
Learn More: How to Handle Claim Denials & Maximize Reimbursements
DENmaar’s Mental Health Medical Billing Service
As you can guess from the article, medical billing for mental health is not a walk in the park. A lot of effort, blood, and sweat goes into the entire process. It can be time-consuming and really frustrating for mental health practitioners who just want to tend to their client’s needs.
Here at DENmaar, we partner with concerned practitioners to offer pre-authorization, third party billing, claims follow-up, and to assist with appeals for any denied insurance claims. With DENmaar, you get the assistance of our medicare behavioral health billing specialists to make your billing process easier than ever. Call us on 844-727-3627 to get started!
Related Posts
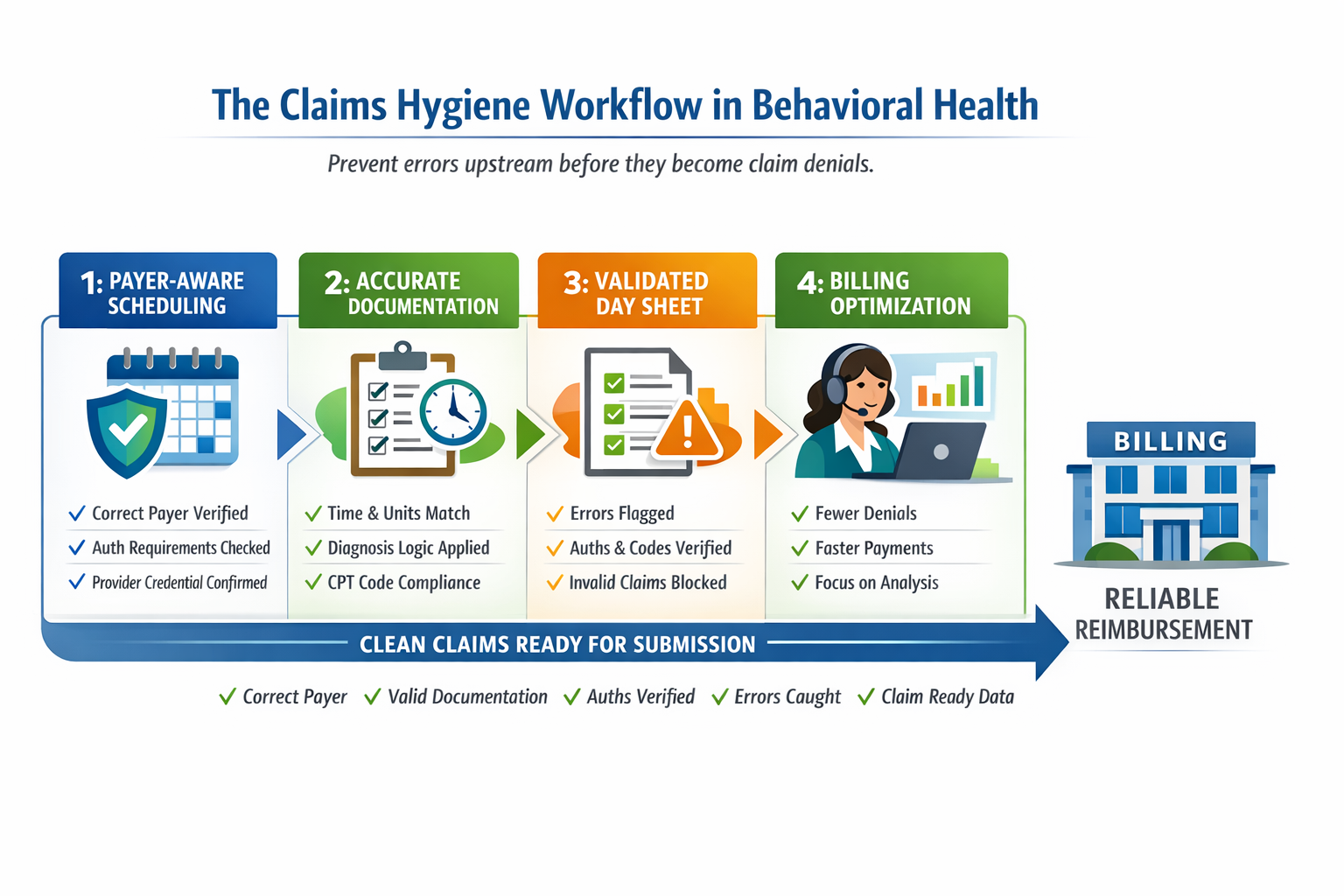
Claims Hygiene: How DENmaar Prevents Rejections Across Therapy, Medication Management, SUD, IOP, and Community-Based Care
In behavioral health billing, most revenue problems do not start with denials....
What “Claims Hygiene” Really Means in Behavioral Health
And Why Most Practices Are Fixing It Too Late Most behavioral health practices...
Guidelines for a Convenient Behavioral Health Medical Billing Process
Medical billing on its own is a seriously complicated process. However, medical...
Avoiding Billing Errors for an Efficient Behavioral Medical Billing Process
Medical billing can be a crucial, but complicated process. It constitutes one of...