Every few months, a new “AI-powered” behavioral health platform promises to revolutionize care. Smarter documentation. Automated billing. Instant insights.
But here’s the truth: AI means nothing without compliance.
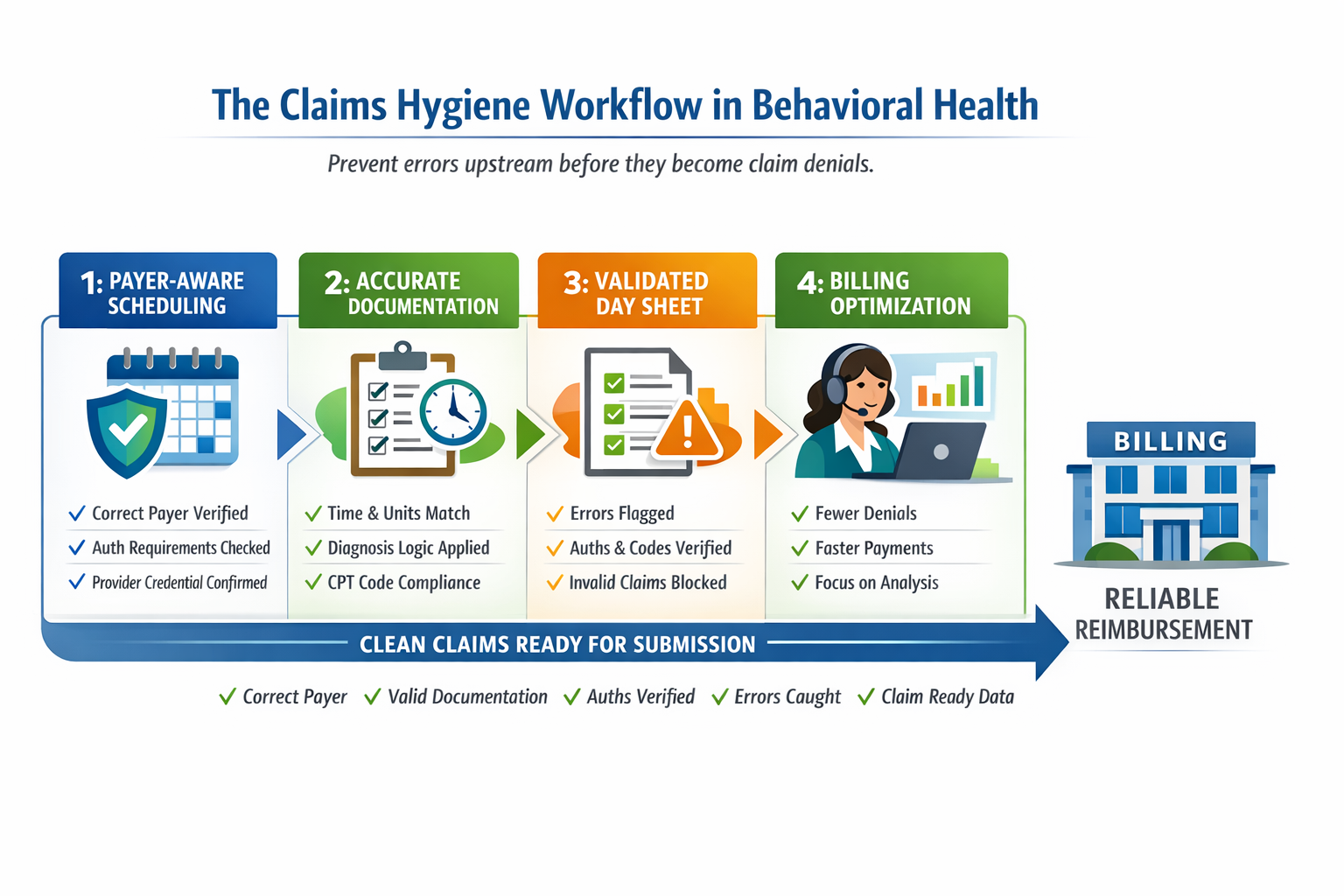
In behavioral healthcare, the systems that last aren’t the flashiest; they’re the ones that understand CMS rules, payer schemas, and the actual structure of care delivery. AI doesn’t fix rejected claims, reconcile CPT modifiers, or align documentation with Medicaid billing logic. Compliance does.
At DENmaar, we’ve learned this firsthand. Building automation into credentialing, billing, and clinical documentation isn’t about replacing people, it’s about protecting practices. A compliant system gives providers confidence that what they write, bill, and submit will stand up to audit and payment review.
AI becomes powerful after that foundation is solid.
That’s when it can:
- Identify missing documentation for medical necessity
- Flag claims that don’t align with payer-specific schemas
- Generate clinically sound progress notes without breaking compliance
- Forecast reimbursements and eligibility trends with real data integrity
Most EHRs skip this step. They automate chaos.
But in behavioral health, the future belongs to those who design for accuracy first, and AI second.
That’s how we build trust — with payers, providers, and patients alike.
The Real Connection Between AI and Compliance
AI in behavioral health works best after compliance frameworks are established. Once automation is aligned with payer logic and clinical standards, it can amplify operational efficiency. For example, DENmaar’s AI Treatment Planning system leverages data integrity and compliance-first design to generate clinically aligned, audit-ready documentation.
The same approach extends to insurance credentialing and billing workflows, where AI can predict errors, manage timelines, and improve reimbursement cycles — but only when built on a foundation of accurate, compliant data.
Learn more about:
Why Compliance Will Always Outlast Technology
In healthcare, trends change fast, from EHR updates to AI documentation engines. But compliance is constant. It governs how claims are submitted, how documentation is reviewed, and how patient data is secured.
When behavioral health platforms skip compliance, they create automation that accelerates errors. The future of sustainable AI lies in systems that protect accuracy, not replace it.
A compliance-first model ensures:
- Accurate claim submissions aligned with payer schemas
- Clinical documentation that meets audit standards
- Financial protection against denials and rejections
- Data integrity that enhances future AI training models