When behavioral health practices describe a tool as a “game changer,” it’s not because of hype — it’s because it changes their daily reality.
That’s exactly what we’ve heard from teams using DENmaar’s Structured Progress Note 3.0 (AI version).
“The note is very sophisticated and references the objectives. We’ve gotten very positive feedback. It’s been described as a game changer and is working very well.”
— Dr. Erin Jenkins Baker, Licensed Psychologist, HSPP, Auxilium Psychological Services
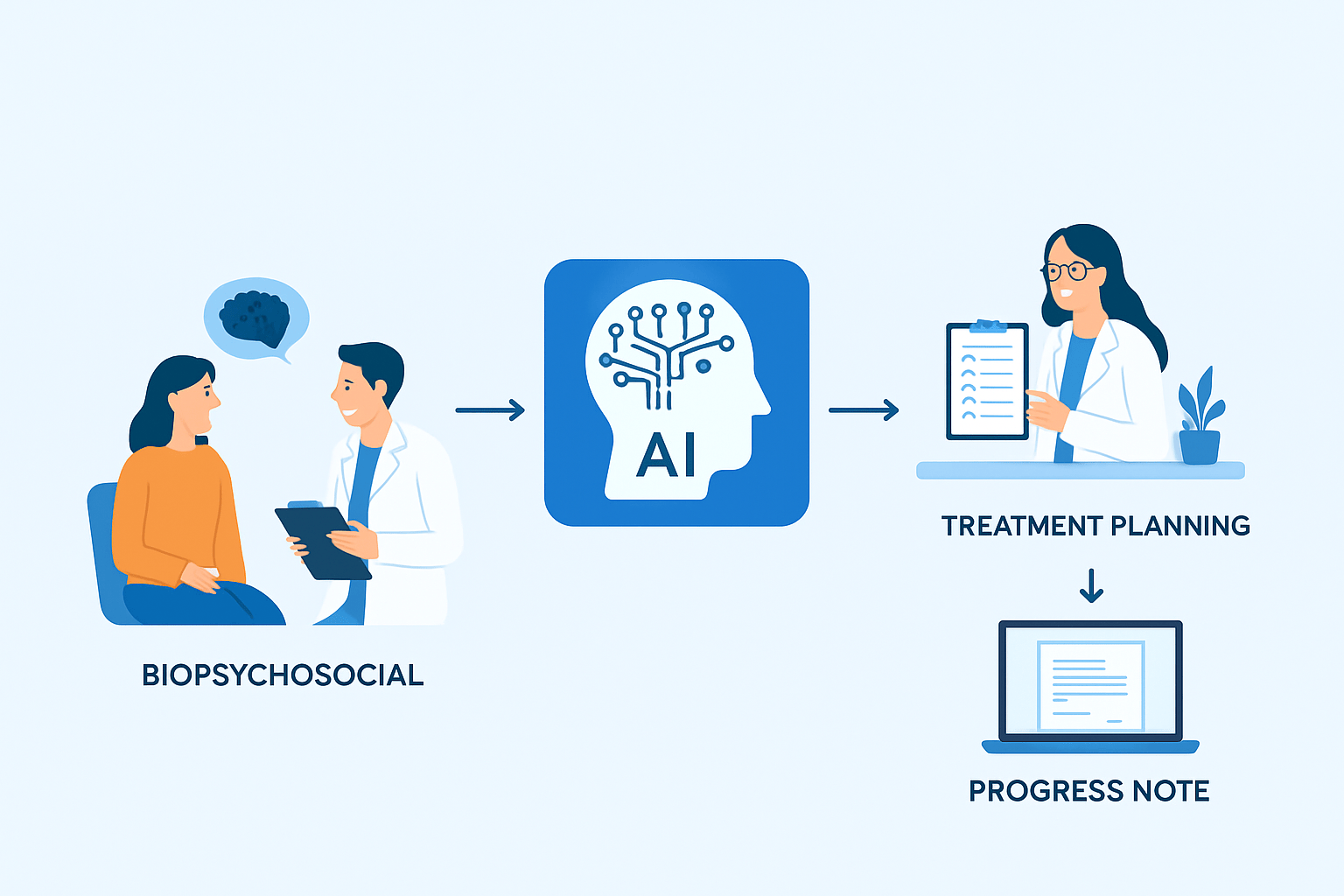
AI That Understands the Clinical Flow
Denmaar AI note doesn’t just generate text — it mirrors how clinicians actually think and document:
- Structured to CMS guidelines: The note follows a logical, CMS-compliant progression of Assessment → Intervention → Progress → Plan, incorporating required medical necessity and measurable objectives.
- Objective-referenced narrative: Each section dynamically references active treatment objectives, ensuring continuity and compliance with supervision and audit standards.
Time-coded alignment: The AI calculates and aligns documentation with CPT-based service parameters, eliminating common audit risks.
The result: notes that are clinically valid, auditor-friendly, and take a fraction of the time.
Explore how our AI-powered EHR software supports compliant, audit-ready documentation.
Saving Hours, Protecting Compliance
Clinicians spend an average of 25–35% of their week on documentation. With AI-driven notes, that time drops by more than half — while accuracy and compliance go up.
DENmaar AI Notes are trained to:
- Recognize clinically relevant interventions based on the session’s type and goals
- Flag missing or inconsistent data points (e.g., objective not referenced, plan not updated)
- Auto-populate recurring patient details while prompting for unique updates required by CMS and payer audits
- Maintain audit-ready structure without sacrificing clinical voice
This means clinicians can sign off faster — and confidently.
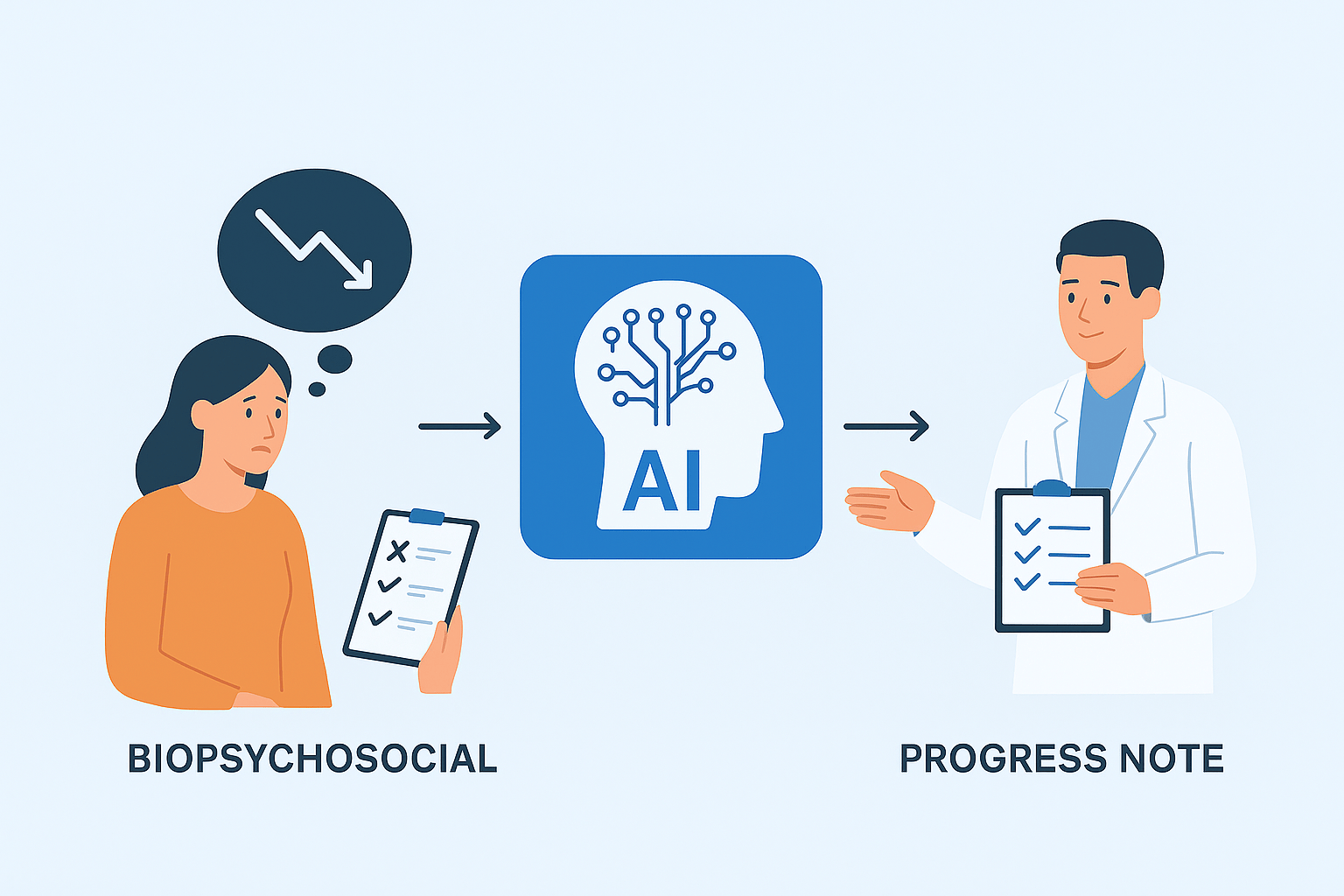
CMS Compliance Built In
Unlike generic AI tools, DENmaar’s documentation engine is rooted in CMS compliance standards for medical necessity, continuity of care, and measurable progress.
Each note includes:
- Objective alignment: Ensuring interventions tie directly to measurable goals
- Medical necessity justification: Automatically summarized in context
- Plan progression tracking: Carrying forward treatment adjustments per CMS’s “ongoing care” expectation
- Supervision-ready structure: Supporting licensed oversight and trainee review requirements
These are the same standards that protect clinicians during audits and sustain payer confidence — without extra effort.
See how DENmaar’s credentialing and billing services help ensure end-to-end compliance.
The New Standard of Throughput
For a growing practice, compliance and efficiency are not opposites. They’re the same goal.
The AI note is not replacing clinicians — it’s removing friction:
- Less typing, more clinical judgment
- Less time explaining compliance, more time delivering care
- Less rework, more revenue through clean documentation
Building Toward $100M in Annual Revenue
Every automation at DENmaar ties back to one mission:
To make behavioral health self-sustaining through intelligent systems that eliminate waste.
AI documentation is one of the most powerful levers toward that future — saving hours per clinician, improving compliance confidence, and accelerating revenue flow.
That’s how we’ll reach $100M:
Not by selling software, but by engineering systems that multiply provider time and compliance integrity.
Conclusion: The Future of Documentation in Behavioral Health
With AI-powered clinical documentation, measurement-based care, and EHR automation, compliance becomes effortless — and productivity thrives.
DENmaar continues to set the standard for mental health EHR software, helping clinicians focus on what matters most: better outcomes and sustainable practice growth.