Yes and That Is Exactly Why It Matters
As behavioral health practices evolve, many eventually ask the same question: Is professional inpatient psychiatry worth supporting?
The short answer is yes, it is a smaller market than outpatient psychiatry. The more important answer is why that does not make it insignificant and why, from a systems and operations perspective, it actually matters more than its raw size suggests.
Organizations evaluating behavioral health EHR platforms built for complex care environments often discover this question late in their growth cycle
The Honest Market Reality
Professional inpatient psychiatry, where a psychiatrist or psychiatric nurse practitioner bills professional services for seeing patients admitted to a hospital, is not a volume driven market.
Compared to outpatient behavioral health:
- There are fewer clinicians
- Fewer billable days per patient
- Less claim volume overall
- Many providers are salaried or hospital employed and never bill independently
If you measure opportunity purely by claim count, it is a small slice of the behavioral health ecosystem. That is the truth.
Why Smaller Does Not Mean Unimportant
Where professional inpatient psychiatry does matter is complexity.
This work sits at the intersection of:
- Hospital workflows
- Daily inpatient evaluation and management billing rules
- Authorization dependencies
- Strict place of service logic
- Discharge day coding requirements
In other words, it is where systems and billing teams break first.
Most outpatient first platforms struggle here because they were not designed to handle:
- One billable encounter per provider per patient per day
- Inpatient evaluation and management code families
- Place of service 21 enforcement
- Discharge day logic
- Hospital credentialing nuances
Supporting this correctly is not about volume. It is about operational maturity.
Practices running into these challenges often encounter limitations in mental health EHR software not designed for inpatient workflows
Higher Friction, Higher Stickiness
Practices that do professional inpatient psychiatry successfully do not switch systems casually.
Why?
- The workflows are fragile
- Billing errors are expensive
- Compliance mistakes create audit exposure
- Re training teams is painful
When a platform does handle this well, it becomes deeply embedded. That creates retention, not churn.
This is especially true when inpatient workflows must align with behavioral health billing services and clean claims management
This Is Rarely A Standalone Business
Almost no one builds a company around only professional inpatient psychiatry.
Instead, it shows up as:
- An extension of an outpatient psychiatry practice
- Hospital rounding for existing patients
- On call or coverage arrangements
- Moonlighting or part time inpatient work
Which means its real value is adjacent, not isolated.
It protects and expands existing practices rather than replacing their core business, particularly for organizations managing psychiatry billing under Medicaid and commercial payers.
Why This Matters for Integrated Platforms
For systems that combine EHR, billing, and operational rules into one environment, professional inpatient psychiatry is a stress test.
If a platform can support:
- Outpatient psychiatry
- Inpatient professional services
- Community based care
- Higher levels of care
- Complex payer rules
It signals something important.
The system was built for growth, not just simplicity.
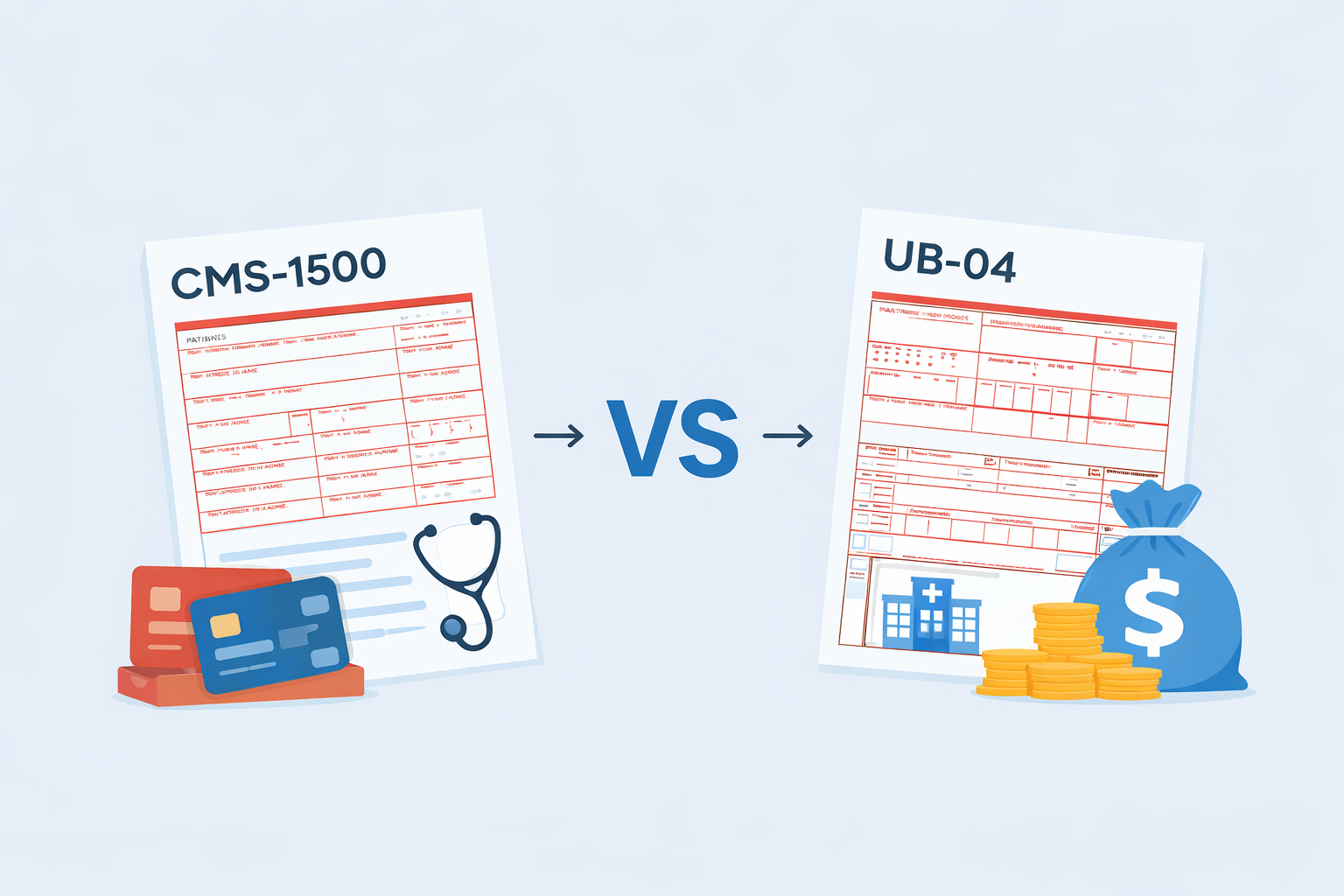
This same logic applies to platforms that can handle CMS 1500 vs UB 04 billing across behavioral health services
The Takeaway
Yes, professional inpatient psychiatry is a small market by volume.
But strategically, it plays an outsized role:
- It hardens systems
- Increases client retention
- Enables practices to grow without switching vendors
- Signals real operational depth
For platforms built to scale with practices, not just onboard them, that matters.
And for practices expanding into more complex care environments, it is often the difference between growth that is sustainable and growth that breaks the backend.
Documentation accuracy and workflow integrity are often reinforced through tools like AI progress notes aligned with inpatient and Medicaid billing logic