Healthcare Revenue Cycle Management is a financial process in which healthcare providers track the patients’ lifecycle from initial registration to the final payment.
RCM makes billing, tracking, and collecting payments from patients efficient. It also minimizes errors and saves time.
The primary aim of revenue cycle management is to improve financial operations.
That’s done by reducing errors and speeding up the process related to revenue generation.
What are the Revenue Cycle Management (RCM) benefits for Healthcare Operations?
There are several benefits that healthcare providers receive from RCM. We are going to discuss the top ones for which RCM is implemented.
Improved Efficiency
After introducing RCM in your healthcare organization, all your revenue-related operations and financial operations become efficient.
It allows healthcare providers to:
- Verify patient insurance
- Take care of billing
- Promptly collect the amount for the services provided
Saves Time and Reduces Cost
Revenue Cycle Management Tools can automate several administrative duties. For instance, staff won’t need to manually handle appointments, send reminders, etc.
Handle Claims Better
The healthcare provider can provide all the required information to the payer. The RCM helps in keeping things clear and avoiding revision and resubmission.
Even then, if the claim isn’t accepted, the insurance providers clearly state the reason for it. It allows the healthcare provider to rectify the issue immediately. Overall, it saves the patient money by making claim handling efficient.
Improved Patient Experience
When there’s a prominent RCM implemented:
- The billing process gets smoother
- The payment processing gets simplified
- Claim approval gets easier
All this makes the overall experience better for sure.
Components and Stages of Healthcare Revenue Cycle
The healthcare revenue cycle consists of multiple stages, and healthcare revenue cycle management must cover all of these to maximize its efficiency.
Pre-registration and Scheduling
You can collect patients’ demographics, such as age and gender, as well as insurance details, to initiate the process even before they arrive. Additionally, RCM includes scheduling patient appointments, ensuring they never miss a visit. When you schedule the appointments reduces no-shows, and merging it with reminders can further improve the turnout rates. Patients will be able to keep their appointments in consideration while planning their schedule.
You can also streamline this process by using a tool like DENmaar to efficiently manage and complete scheduling tasks. Ultimately, as the turnouts improve, it has a positive impact on the other stages of the RCM by making it easier to verify insurance coverage, submit claims, and receive payment.
Registration
This includes general patient information along with the medical history to ensure tailored treatment.
Verifying insurance coverage
The medical provider communicates with the insurance provider. It’s done to verify the correctness of the details provided by the patient and get the necessary approval.
Documenting services and their respective billing codes
All the services and procedures performed have a predefined billing code.
Under this step:
- Everything is documented
- Translated into the billing codes
- Shared with the insurance provider for the claim
The billing codes define how much a healthcare provider will be reimbursed against every service and procedure.
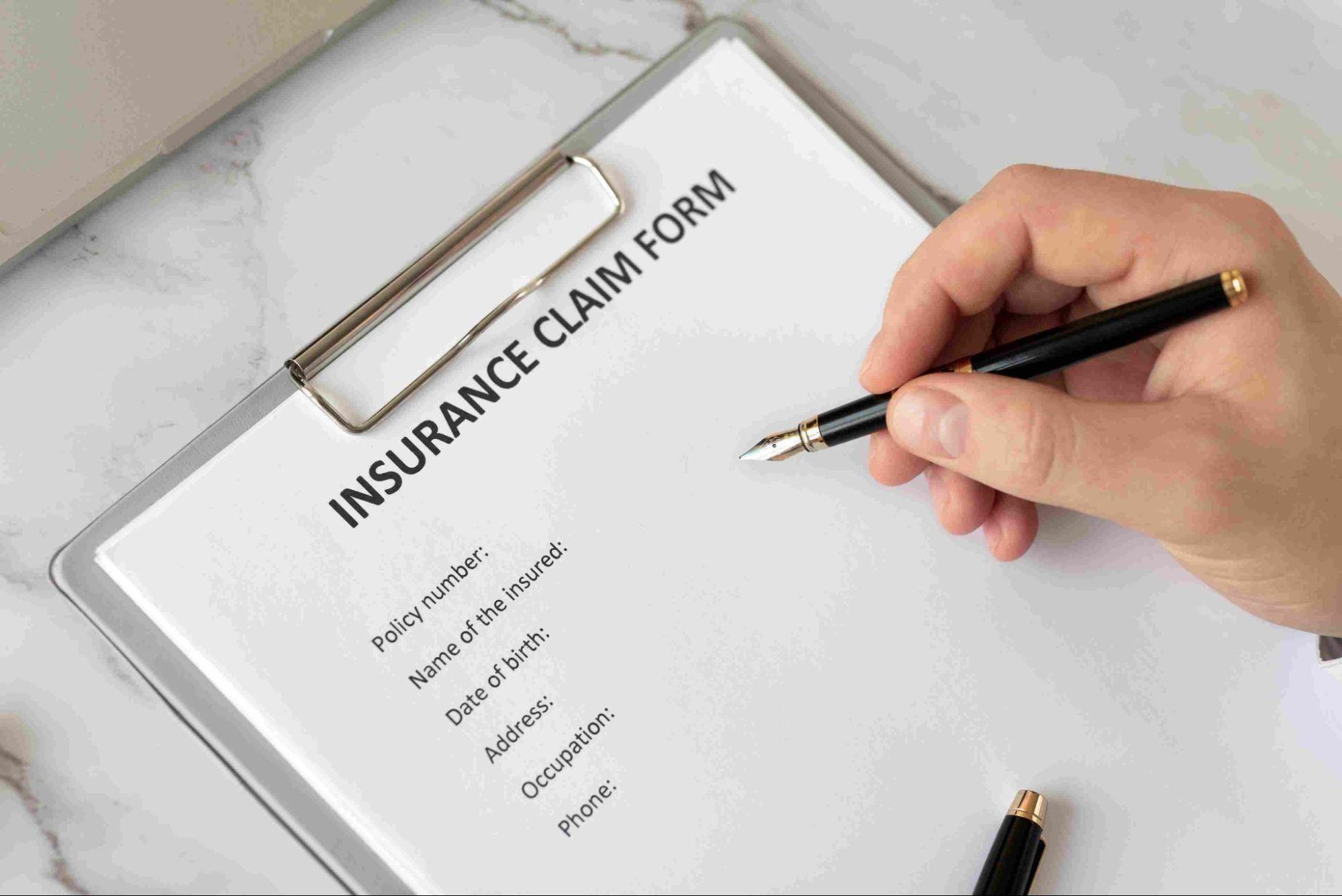
Submitting an insurance claim
After you submit the insurance claim to the provider, they will check all the codes. It’s done to see whether they align with the terms and conditions or not. Based on that, the provider decides how much payment they need to make or entirely deny the claim.
Claim denial management
In case the claim is denied, the payer will mention the reason. It allows the healthcare provider to check the issue and rectify it if possible. Between 5% and 10% of healthcare claims are rejected every year, causing a loss of up to $262 billion. You can avoid your loss with optimized RCM.
Claim payment
Payment is made by the payer is added to the patient’s account by the healthcare provider.
Patient billing
You need to bill the patients if there are any services and procedures that:
- Can’t be added to the claim
- For which the claim is denied
Collecting the pending amount
Once you submit the payment request to the clients, you may require following up and sending payment reminders.
Generating reports
Reporting is essential to understand the overall performance of RCM. It gives access to various key performance indicators and identifies room for improvement for each stage.
Best Practices of Revenue Cycle Management
There are several best practices that help you bring out the best in your healthcare revenue cycle management process. We have listed the important ones here:
- The data collection should be comprehensive and accurate. You must collect personal information, medical history, and insurance details accurately through digital tools to speed up the process while minimizing errors.
- Use a real-time verification app to verify the patient’s insurance details. It will ensure that the patient is eligible for the claim, which reduces claim rejections.
- Stay compliant by strictly following all relevant laws and regulatory requirements. Safeguard yourself from legal issues and penalties.
- Healthcare providers must conduct proper training regarding all stages of the RCM.
- Keep your staff updated regarding the code information. Let them know if there are any changes. They must know how to document accurate codes to avoid claim denials and resubmissions. You must provide an additional check on overall claim submission. You can use automated claim-scrubbing tools for this purpose. They will help you identify and correct data-entry errors.
- There must be a robust tracking system to check the real-time status of submitted claims. It will also help your staff to address denials promptly. This ensures that the revenue streams stay uninterrupted.
- There should be transparent patient communication. You must provide them with a complete overview of the costing, procedure, and payment-related aspects.
- The billing and payment process should be easy for customers. Give them detailed bills so that they can understand why they are charged. You must also provide them with multiple payment processing options, making things flexible for them.
- Use SaaS based applications such as DENmaar to simplify revenue cycle management. It also helps you automate manual tasks and reduce human errors.
- You must regularly check the performance of your revenue management cycle. Checking insights for every stage will help you improve the process.
How Revenue Cycle Management Process Affect Revenue?
In this section, we will examine how each stage contributes to minimizing costs and optimizing revenue.
RCM Stage | Its Effect on Revenue |
Pre-registration | Accurate pre-registration saves patients’ time, improving the overall experience and leading to trustworthy engagement, affecting revenue. |
Patient registration | RCM improves accuracy, minimizing claim denials and billing issues. Hence, reducing the overall costs. |
Claim Management | Manually handling communication regarding insurance claims can lead to more time due to inaccuracy. However, RCM ensures timely claim processing with minimal back-and-forth. This optimizes revenue by saving staff time and rapid reimbursement. |
Billing and Payments | RCM allows you to share detailed billing and payment obligations. It develops transparency, encouraging clients to comply with their payment obligations faster and hence improving the revenue. |
Reporting and Analytics | It allows you to find areas of improvement, which directly improve various stages, and finally, make a positive impact on the revenue. |
Stay Compliant | One of the biggest perks of revenue cycle management is avoiding compliance and legal issues. When you stay compliant, you save on penalties, and in one way, it’s optimizing revenue. |
How DENmaar Can Provide You with Efficient Healthcare Revenue Cycle Management?
DENmaar is a unified platform that helps healthcare providers and mental health specialists streamline their administrative tasks and billing process. With DENmaar having your back, you can significantly optimize your healthcare revenue cycle management. It will help you digitalise the information collection and patient registration.
Free RCM Software and Expert Claims Handling
DENmaar gives you FREE access to its powerful RCM software. Unlike other solutions that only offer software, Denmaar’s offers much more.
Our dedicated Expect Claim Management team handles claims issues. We deliver tailored solutions that tackle complex claim challenges head-on, helping reduce denials, speed up reimbursements, and significantly boost collections and revenue.
It makes it easier to communicate with the insurance provider and manage the claims.
The All-in-One Advantages that You Only Get with DENmaar
Even the overall billing and payment processing can be handled through DENmaar. Therefore, it’s your go-to tool when you want to improve RCM without juggling between multiple apps.
We offers a truly all-in-one solution that combines expert services with free software, simplifying your operations, reducing vendor complexity, and ultimately producing a better outcome for your practice.