In behavioral health, documentation is both essential and exhausting. Clinicians spend hours each week completing biopsychosocial assessments, building treatment plans, and writing progress notes — all while balancing packed schedules and rising administrative demands from payers and regulators.
The problem isn’t the work itself.
It’s the friction between each step of the clinical documentation process.
AI is finally solving that.
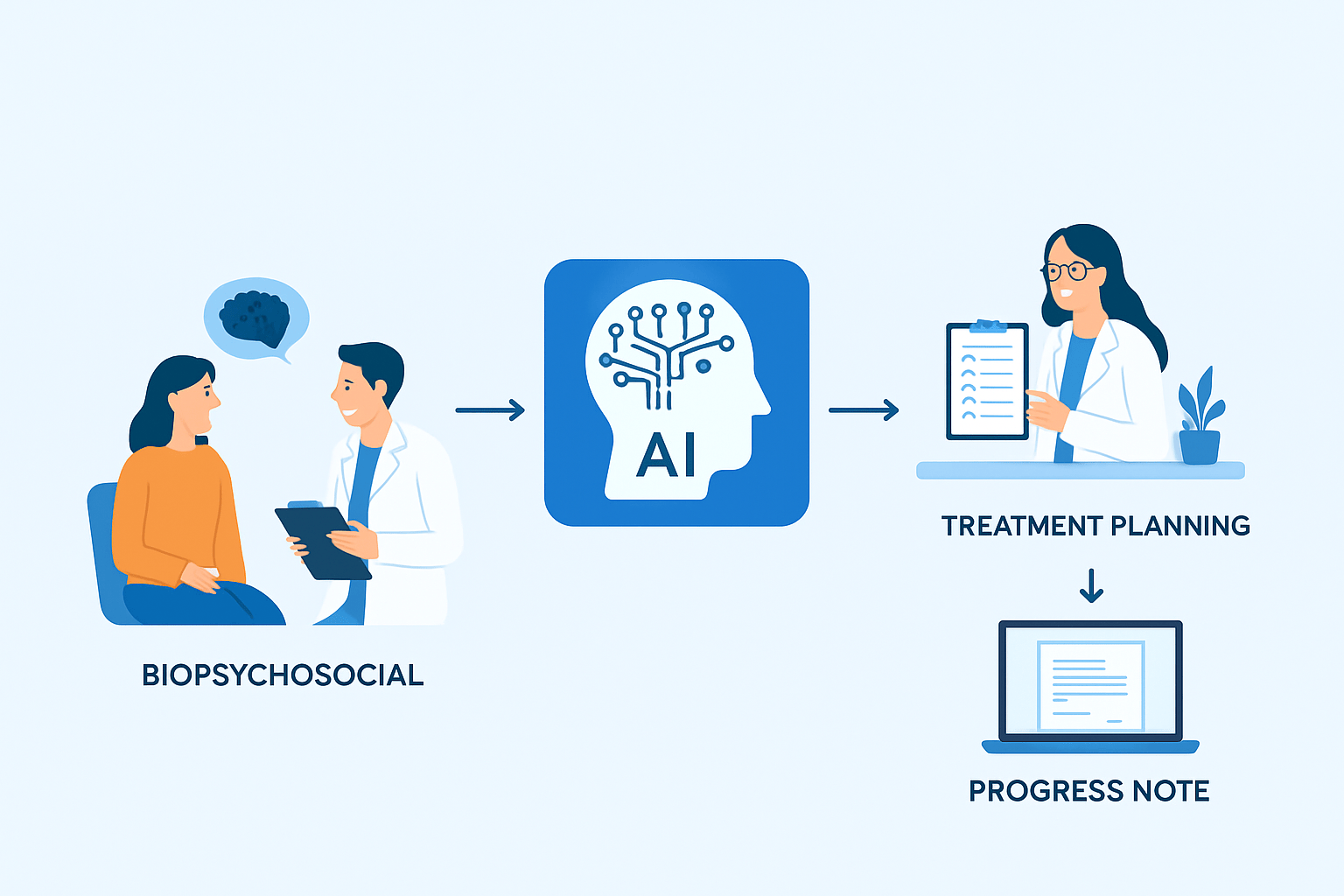
Today, advanced behavioral-health AI systems are connecting the full clinical workflow into a streamlined, intelligent sequence:
Biopsychosocial → Treatment Plan → Progress Note
— reducing documentation time, improving accuracy, and helping practices stay compliant without burying clinicians in paperwork.
Here’s how.
1. AI Enhances the Biopsychosocial Assessment
The biopsychosocial (BPS) drives the clinical picture — symptoms, history, social factors, risk level, functional impact, and strengths.
But historically, clinicians have faced:
- Repetitive questions
- Manual data entry
- Long narrative sections
- Difficulty synthesizing all information into a clear profile
AI changes this by:
-
Automatically summarizing patient narrative
AI can take the raw client responses and generate accurate, structured summaries that fit Medicaid and CMS expectations.
-
Identifying core clinical themes
AI surfaces common threads across symptoms, history, and psychosocial factors — helping clinicians rapidly understand the case.
-
Pre-populating treatment plan problem areas
Instead of starting from scratch, the clinician begins with a smart draft rooted in the actual BPS data.
Result:
What once took 45–60 minutes is reduced to 10–15 minutes with better accuracy and consistency.
2. AI Bridges Directly Into the Treatment Plan
This is where AI has created the biggest breakthrough.
Historically, treatment plans fail because they are:
- Generic
- Not tied to assessment data
- Not measurable
- Not updated consistently
- Out of alignment with payer expectations
AI now links the treatment plan directly to the BPS.
-
AI suggests problem statements
Based on risk, symptoms, and functioning, AI creates patient-specific problem statements.
-
AI generates measurable goals and objectives
These are tied to best practices for therapy, psychiatric care, or SUD services.
Everything stays in CMS and Medicaid-compliant language.
-
AI matches evidence-based interventions
CBT, ACT, DBT, EMDR, MAT, relapse prevention — whatever fits the case — are auto-suggested with correct phrasing.
-
AI maintains continuity
When the clinician updates a goal, the AI updates related interventions and notes across the chart.
This creates a massive win:
Consistency from intake → goal-setting → progress notes.
For a deeper look at AI-powered treatment planning, explore DENmaar’s article:
AI Treatment Planning in Behavioral Health
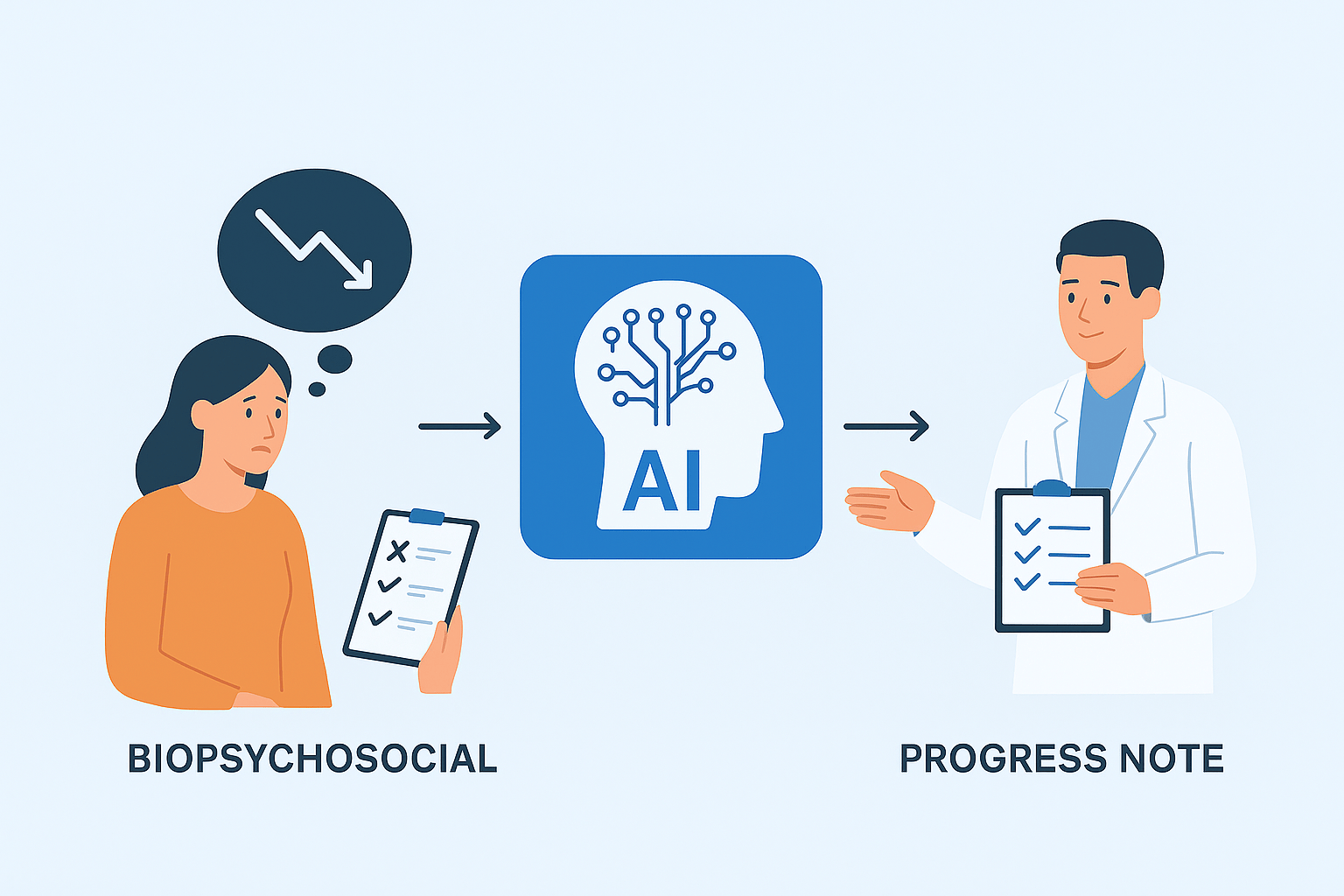
3. AI Powers Progress Notes With True Clinical Continuity
Progress notes have always been the most repetitive part of documentation. Clinicians repeat information across dozens of sessions.
AI ends the redundancy by linking directly to the treatment plan and prior notes.
-
AI pulls goals + objectives into the note
The note dynamically displays the relevant treatment plan content.
-
AI suggests interventions based on the plan
Every session stays aligned with measurable objectives.
-
AI creates a first-draft note instantly
Clinicians then edit for accuracy — saving an average of 5–12 minutes per note.
-
AI flags missing elements for compliance
Time, modality, interventions, response, risk — everything required for CMS, Medicaid, and commercial payers is checked automatically.
Accuracy goes up. Time goes down. Compliance becomes easier.
Learn more about compliance-focused AI workflows here:
AI and Compliance in Behavioral Health
4. Speed + Efficiency + Accuracy = Better Care
When AI handles the repetitive structure of documentation, clinicians reclaim time and clarity.
Here’s what practices are reporting:
- 40–60% faster documentation cycle
Especially across progress notes and treatment plans.
- Improved MBC tracking and outcomes
Because goals, symptoms, and notes stay aligned week to week.
- Fewer payer issues
AI reduces documentation errors, improving clean-claim rates and lowering the risk of recoupments.
- Better coordination across providers
Notes, goals, and assessments stay consistent across therapy, psychiatry, and SUD teams.
- Most important: less burnout
Clinicians spend more time with patients and less time typing.
For additional payer-facing improvements, explore DENmaar’s billing solutions:
Behavioral & Mental Health Billing Services
5. The Future: Fully Connected Clinical Documentation
The industry is shifting toward agentic AI — systems that don’t just help clinicians document but actively ensure clinical coherence.
Within the next 24 months, practices will expect:
- Automated assessment scoring
- Reactive updates to treatment plans based on symptoms or risk
- AI-driven continuity that identifies when goals are met
- Intelligent recommendations for level of care changes
- Compliance engines that adjust to state-specific Medicaid rules
This is where platforms like DENmaar are headed:
A completely unified intake → BPS → treatment planning → progress note flow supported by AI.
To keep your practice fully credentialed and payer-ready, explore:
DENmaar Insurance Credentialing Services
Conclusion
AI isn’t replacing clinicians.
It’s replacing the inefficient documentation process that has slowed them down for decades.
By linking the BPS, treatment plan, and progress note into one seamless, intelligent workflow, AI is giving clinicians back time, clarity, and confidence — and helping practices operate at a level of efficiency that simply wasn’t possible before.
This is the future of behavioral health documentation:
Faster. More accurate. Fully connected. And powered by AI.