In behavioral healthcare, one of the greatest inefficiencies happens in the gap between a patient’s intake, their treatment plan, and the progress notes that follow. Every provider knows that consistency, documentation accuracy, and clinical compliance are critical — yet many systems silo these steps, forcing clinicians to repeat data entry and lose valuable clinical context along the way.
At DENmaar, we’re changing that with AI-powered treatment planning software designed for behavioral health professionals.
Building Intelligence Into the Golden Thread
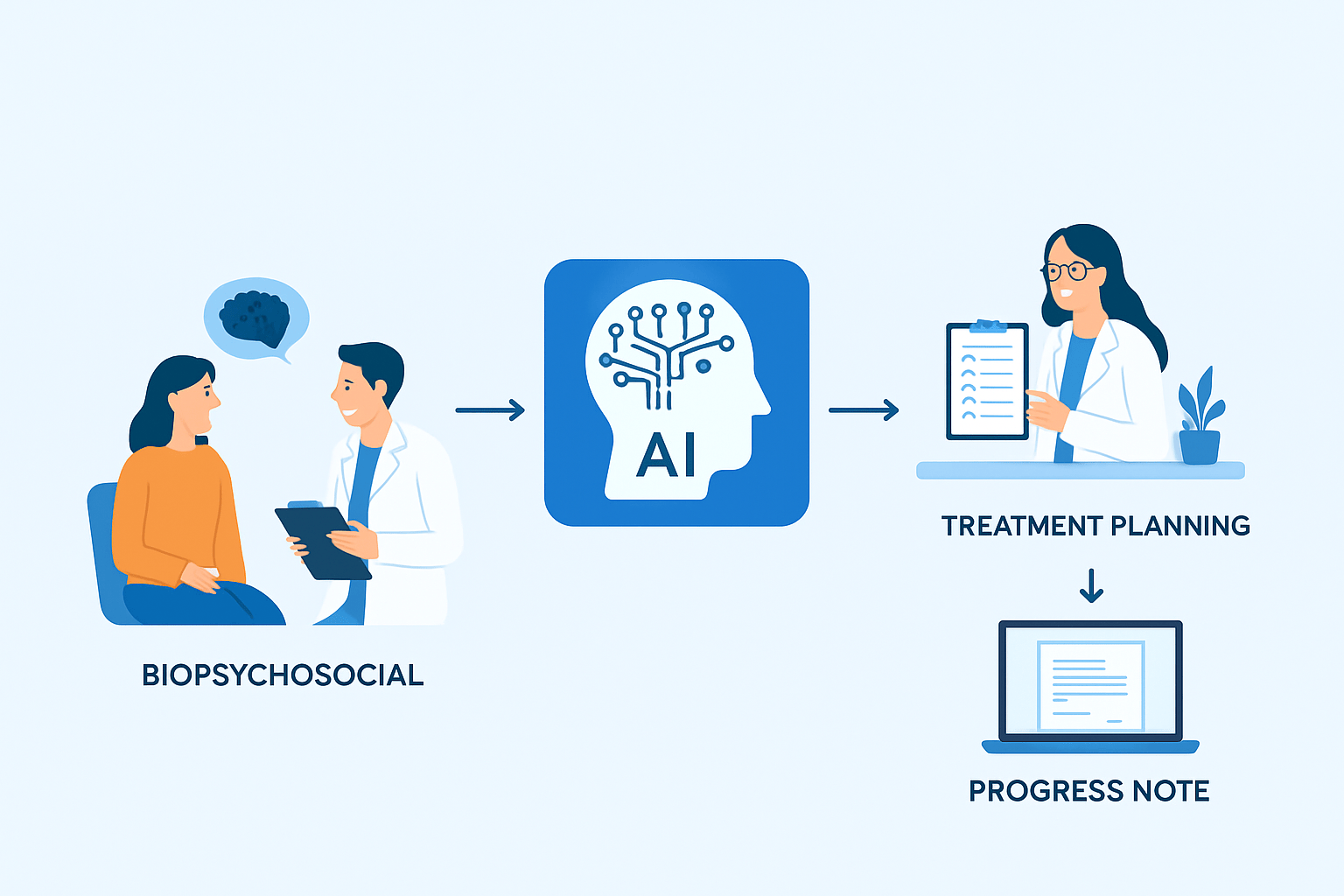
Our upcoming AI-driven treatment planning engine bridges the full “Golden Thread” of care — from the initial biopsychosocial assessment to the treatment plan and each progress note thereafter.
When a new patient is onboarded, clinicians or intake staff complete a biopsychosocial that captures the person’s history, risk factors, strengths, and presenting issues.
DENmaar’s AI for behavioral health then translates that information into a clinically structured treatment plan — automatically generating goals, objectives, and interventions tailored to the diagnosis and patient narrative.
Each subsequent progress note intelligently references those treatment goals, allowing providers to document progress with precision while maintaining CMS and insurance compliance.
How AI Treatment Planning Works
1. Intake: From Data to Structure
A patient’s biopsychosocial becomes structured data — not static text. The AI parses key domains such as presenting problems, history, strengths, and risks.
2. Treatment Plan Creation
DENmaar’s AI-powered treatment planning software suggests SMART goals, measurable objectives, and evidence-based interventions that clinicians can review and approve. No more writing plans from scratch — only refining and personalizing them.
3. Progress Note Integration
When writing notes, the system automatically surfaces relevant treatment objectives, MBC scores (like PHQ-9 or GAD-7), and goal progress. Providers can document with full context, reducing note time by over 50%.
Explore how our AI clinical notes system links treatment plans to documentation and supports audit-ready compliance.
4. Continuous Learning & Insights
As more data accumulates, the AI becomes smarter — recommending updated interventions, flagging stalled progress, and syncing insights directly with outcome tracking dashboards.
Rolling Out Across Therapy, Psychiatry, and SUD
We’re implementing this technology in phases to ensure clinical precision and behavioral health compliance:
- Therapy: Automating plan-to-note linkage and embedding Measurement-Based Care (MBC) outcomes tracking.
- Psychiatry: Expanding to include medication management, mental status exams, and outcome correlation.
- Substance Use Disorder (SUD): Integrating ASAM dimensions, relapse-prevention metrics, and group-session analytics.
Each phase builds on the previous one, creating a unified ecosystem that supports multi-provider behavioral health practices from intake to billing.
Check out how DENmaar’s full range of practice management and EHR solutions span intake, billing, documentation and beyond.
Why AI-Driven Treatment Planning Matters
This innovation isn’t just about efficiency — it’s about better patient care.
When clinicians spend less time typing and more time understanding, patients benefit. And when treatment plans are directly tied to measurable outcomes, payers and providers finally share the same language of progress.
At DENmaar, our mission is to create a behavioral health platform where clinical documentation, billing, and AI intelligence work in harmony.
See how our AI-enhanced progress notes help therapists capture and report outcomes with precision and speed.
The result: a faster, smarter, and more connected path to patient success.