Streamlined, Affordable, and Fully Integrated
with Billing + Free EHR
Insurance Credentialing for
Mental Health Providers



Credentialing That Builds Your Practice
DENmaar offers two tailored credentialing programs to get you in-network and generating revenue — fast.
Whether you’re launching or expanding, we handle the process from start to finish.
CoreFour Credentialing
Perfect for solo or group providers starting fresh
Get credentialed with the four commercial payers that cover 95% of claims:
- Aetna
- Cigna
- Blue Cross Blue Shield
- United Healthcare
Includes:
- Full application and follow-up for each payer
- DENmaar EHR/RCM with Credentialing module included
- Credentialing may complete in as little as 30 days
- Flat rate: $1,000 per provider
- EIN and Type 2 NPI required
Credentialing Expansion
For practices adding providers or joining more networks
Already up and running?
DENmaar can help you grow:
- Add new providers to current payer contracts
- Apply to Medicaid, Medicare, or additional commercial plans
- Reattestation, CAQH updates, and state-specific filings
- Custom pricing based on your needs
- Available only to active DENmaar billing/system users
Why DENmaar?
- 20+ years focused on Behavioral Health & MHSA
- In-house insurance, billing, and credentialing team
- Fully integrated
EHR and RCM system - Transparent pricing
— no hidden fees
What You Get with
DENmaar Credentialing

Application processing for all
major insurance payers

CAQH setup and
ongoing re-attestation

Follow-up with payer panels
and status updates

Integrated support with our
billing and claims team

Seamless EHR access (telehealth,
AI notes, eRx, clearinghouse
fees—included)

Start Seeing Clients.
We’ll Handle the Payers.
- At DENmaar, we make credentialing simple. We don’t just help you get paneled—we plug you into a complete system designed for behavioral and mental health practices.
- Our credentialing is not a stand-alone service. It’s the first step in getting your practice up and running on our insurance billing platform and free EHR/RCM —so you can focus on care, not paperwork.
Why It Works:
A Fully Connected System
- Unlike other services, we don’t offer credentialing in isolation. Our strength lies in connecting credentialing directly to our billing services and free EHR platform.
- That means fewer delays, better follow-through, and a smoother path from credentialing to claims submission—and getting paid.
From Credentialing to Outcomes-Based Billing
— All in One System
With DENmaar, credentialing is just the beginning. Once enrolled with payers, providers are activated into a fully connected
EHR / RCM platform that supports modern, outcomes-driven care — including automated clinical assessments like PHQ-9
and GAD-7, and billing for CPT 96127.
Credentialing
We manage your provider enrollment with insurance panels from start to finish — including Medicaid and commercial payers.
Insurance
Alignment
Our billing team confirms which assessments and services (like CPT 96127) are billable per payer — no guesswork, no rejections.
Outcomes Engine
Activation
Providers gain access to DENmaar’s Outcomes Engine — delivering and scoring PHQ-9 and GAD-7 directly through the EHR or patient portal.
Automated
Documentation + Billing
Scores are auto-inserted into progress notes and trigger 96127 billing — up to 4 units/month per patient — fully tied into the claim cycle.
The result? Your practice is credentialed, outcomes are measured, documentation is compliant, and claims are submitted
— all in a single, integrated system.
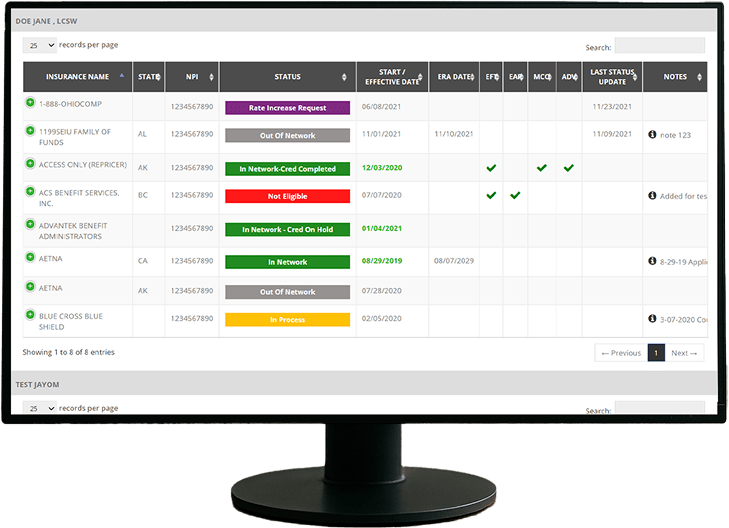
Credentialing Management Software:
Easily track, update, and manage provider credentialing statuses across multiple insurance networks with our intuitive
software. This centralized interface displays real-time updates on eligibility, effective dates, and payer-specific statuses
—ensuring accuracy, transparency, and streamlined communication in your credentialing workflow.
Simple,
Transparent Pricing

One-time credentialing
fee per provider
(for all applications)

Monthly follow-up fee
for active management
and re-attestations

No software charges – EHR
is included when you
use our billing services

Bundle pricing available
for group practices
We only offer credentialing as part of our billing + EHR ecosystem. That’s how we ensure you get the results you need.
TESTIMONIALS
WHAT OUR
CLIENTS SAY

I referred one of my colleagues Dr Aaron to you he is just starting g his psychology private practice and looking at where to start. I told him hands down you guys are the best billers and have a great EMR and team. He said he reached out just wanted to let you know!

Nicole Lightman, PhD
Clinical Psychologist
FANTASTIC job keeping things rolling along with any and all of our billing concerns as well as responding to other issues which may well have been out of your wheelhouse. We are VERY grateful to have you and the crew in our corner.

Kings and Queens Family Services
I appreciate you all so much and DENmaar has been such a blessing Donna to our overall operations and success as an expanding company—allowing us to ultimately operate more efficiently, get our claims paid more consistently, ad stay on top of the critical credentialing piece, among other things. Teamwork does in fact, make the dream work. I’ll loop Chris/Isabella in on this message thread too, as I want All of your team to be aware of how much we appreciate our working relationship with DENmaar

Jenny at Caring Center
Thank you for your diligence!! I appreciate it so much. Thank you Edwina…

Michelle Heller, M.S, LPC, CCATP Owner at Hope In Motion, PLLC
Thank you so much Amy! I will be referring to DENmaar as often as I am asked about credentialing services.

Monet Counseling Service
Frequently Asked Questions
What is insurance credentialing?
Insurance credentialing is a process wherein healthcare providers apply to health insurance companies to be a part of their provider network. This process involves the verification of a healthcare provider’s credentials and understanding the credentialing in healthcare before they are enrolled into their network.
How long does Insurance Credentialing take?
Insurance Credentialing is a long and intricate process. Typically, the entire payer credentialing process can take anywhere from 90 to 120 days to conclude.
How to get Insurance Credentialing?
To get health insurance credentialing, approach the insurance company whose network you’d like to join. Follow the credentialing process for providers as instructed by them and follow up with the company until your application is either accepted or denied. To increase your chances of succeeding, we suggest you seek the assistance of a professional insurance credentialing specialist.
What services does DENmaar offer to facilitate insurance credentialing?
DENmaar provides comprehensive support including automated updates on credentialing status, assistance with documentation, and help with appeals for panel closures.
How does DENmaar's automation benefit the credentialing process?
DENmaar’s automated systems keep providers informed about application status, expiring documents, and facilitate quick updates to ensure smooth and efficient credentialing.
How does DENmaar's automation benefit the credentialing process?
Yes, DENmaar assists with appeals against claims denials and panel closures, ensuring providers have the best chance to be accepted into insurance panels.



